Alzheimer's and Related Dementias: Support for Montana Farmers and Ranchers and their Families (Volume 2)
Publication 4642
Reviewers
The authors express appreciation to the following individuals for reviewing one or more articles and for making suggestions for improvement.
- Nancy Anderson, Outreach Director, Volunteer Program Manager, AARP Montana, Helena
- Walt Anseth, Rural Development, Farm & Ranch Loan Manager, Montana Department of Agriculture, Helena
- Renee Brooksbank, Esq, MTGEC Associate Director, Montana Geriatric Education Center, University of Montana, Missoula
- Pat Coon, Physician, retired; The Montana Alzheimer’s and Dementia Coalition, MD
- Jennifer Erickson, Branch Manager/Relationship Manager, AgWest Farm Credit
- Todd Kesner, former Director, 4-H Center for Youth Development MSU Bozeman
- Kaleena Miller, Madison/Jefferson County MSU Extension Agent, Whitehall
- Tyson Miller, Deputy Bureau Chief, Montana Motor Vehicle Division, Helena
- Betty Mullette, The Montana Alzheimer’s and Dementia Coalition, Billings
- Ken Nelson, McCone County MSU Extension Agent, retired
- Gary A. Peterson, Alzheimer’s caregiver, Bozeman
- Jackie Pondolfino, Park County MSU Extension Agent, Livingston
- Kimberly Richardson, Ravalli County MSU Extension Agent, Hamilton
- Emily Scruggs, Lewis and Clark County MSU Extension Agent, Helena
- Jan Smith, retired Big Sky Senior Services, Montana Alzheimer’s and Related Dementia Coalition, Billings
- Michael Walker, Bureau Chief, Montana Motor Vehicle Division, Helena
- Jo Ann Warner, Associate Director, Western Extension Risk Management Education Center, Washington State University, Pullman
- Sue Warren, RN, MSN, Great Falls Area volunteer, Alzheimer's Association--Montana, Great Falls
- Wendy Wedum, Pondera County MSU Extension Agent, Conrad.
Contributors
The authors express appreciation to the following individuals for sharing examples of Alzheimer’s situations and stories for articles: Walt Anseth, Nora Brunner, Jennifer Erickson, Robert E. Lee, Carrie Sue Lerum, Ken Nelson, Cathy Ratzburg, Bobbie Roos, Mike Schultz, Roubie Younkin.
The design and printing of this publication is funded in part by a generous contribution from the University of Montana Geriatric Education Center, Western Extension Risk Management Education, AgWest Farm Credit, and AARP Montana.
 |
 |
 |
 |
 |
 |
The design and printing of this publication is funded in part by a generous contribution
from AARP Montana, AgWest Farm Credit, Western
Extension Risk Management Education, Montana Farmers Union, and the University of
Montana Geriatric Education Center.
Photo: Lisa Terry
Authors
- Marsha A. Goetting, PhD, CFP®, CFCS, Professor and MSU Extension Family Economics Specialist, Department of Agricultural Economics and Economics
- Vicki Schmall, PhD, Emerita Professor and Extension Gerontology Specialist, Oregon State University
- S. Dee Jepsen, PhD, Professor and Extension Agricultural Safety and Health State Leader, The Ohio State University
- Jennifer Munter, MS, former graduate student, MSU Department of Health and Human Development, now Assistant Director, MSU Extension Nutrition Education Program
- E. Edwin Eck, Emeritus Professor, Alexander Blewett III School of Law, University of Montana
Dedication
BEING NOMINATED TO THE MONTANA ALZHEIMER’S and Related Dementias Workgroup (now Coalition) in 2016 was an honor. As of 2024,
the coalition is going strong with quarterly meetings via Zoom. Often more than 25
members of the coalition attend from state agencies, community organizations, educational
institutions, as well as individual volunteers, who are all dedicated to improving
Montana’s response to the growing number of people with Alzheimer’s and related dementias.
These professionals and volunteers have taught me so much about Alzheimer’s and related
dementias. Volume 2 of this magazine is dedicated to these “Montana treasures.”
This volume is also dedicated to a special couple, Nora and Rod Brunner of Bozeman
whom I met because they were friends of my husband. Rodney “Rod” Brunner grew up on
a family farm near Power, Montana. He recalled the joys and hardships of farm life.
He remembered seeing winter snow coming through the loose windows in the bedroom in
which he and his brother slept. Rod served our country in the U.S. Army from 1969
until 1971. He was awarded the Purple Heart Medal for combat wounds he received during
the Vietnam War. On October 14, 1978, Rod married the love of his life, Nora Bellows
Larson. Rod had a successful career in the Department of Labor and Industry as a Programs
Supervisor. He was also a board member and on the finance committee of the Help Center
in Bozeman. In his free time, he loved fly fishing with his pal Larry, camping, hanging
out at the cabin with “pard” Gary, golfing, and tying flies.
In 2009 Rod was diagnosed with Alzheimer’s. Because of experiences with my mother,
who had Alzheimer’s, I could predict the progression of the disease
and the future challenges for Nora and Rod. In some ways, the diagnosis was not a
surprise, as his mom, Verena Asmus Brunner, passed away from Alzheimer’s in 2010.
Nora became Rod’s compassionate and nurturing caregiver as the disease progressed.
She was always there for him and was devoted to making his Alzheimer’s journey meaningful.
During the later years, his “pards,” Larry Cloninger and Gary Peterson, visited him
every Tuesday to relive their past escapades and talk politics. Rod always had a smile
even at the end. All who knew them have the utmost respect for Nora and Rod’s bravery
throughout their Alzheimer’s journey. Rod, we miss you.
Marsha Anderson Goetting
The authors designed Volume 1 and 2 to reach Montana agricultural producers facing early to middle stages of Alzheimer’s and their families with information that can make a positive difference in their lives.
Volume 1 explores these topics:
- Agricultural Occupations and Alzheimer’s: Potential Causes, Signs, and Early Diagnosis
- Alzheimer’s and other Dementias: NOT a Normal Part of Aging
- Progression of Alzheimer’s
- Alzheimer’s and Caregiver Wellness
- Communicating about an Alzheimer’s Diagnosis
- Hope for the Future: Treatments or a Cure for Alzheimer’s?
If you would like to receive a free copy of Volume 1 of the magazine, contact a local MSU Extension office or email marsha.goetting@montana.edu.
Alzheimers and Driving: Concerns and Decisions
WHEN A FARMER OR RANCHER BEGINS SHOWING signs of Alzheimer’s, the question is not if they should stop driving, but rather
when. Safe driving requires the ability to pay attention, concentrate, respond quickly,
and make correct decisions. Early signs of Alzheimer’s may not mean a farmer or rancher
can no longer drive. Some individuals – although not all – may be able to drive safely
for a limited time.
Driving is a complex task
Alzheimer’s is progressive, which means memory, visual-spatial orientation, cognition,
and other brain functions become worse over time. As a result, a person’s driving
skills will decline. At some point, they will no longer be safe behind the wheel.
Eventually, a farmer or rancher will have to give up driving any vehicle, whether
it be a car, truck, 4-wheeler, tractor, combine, hay baler, or swather. Driving on
back country roads may no longer be possible because of safety issues and the potential
for getting lost.
Friends and family members are often the first to notice signs of unsafe driving.
Passengers, neighbors, and others may also express concerns about the person’s driving.
Because the progression of Alzheimer’s varies from person to person, knowing when
a farmer or rancher should no longer drive is difficult. Carefully watch their driving
and be aware of signs of unsafe driving.
Montana rules about medical conditions and driving
Montana is not a mandatory reporting state. This means medical professionals do not
have to report to the Motor Vehicle Division (MVD) if a driver suffers from a medical
or health condition that may affect their ability to safely drive a vehicle. However,
when applying for or renewing a driver’s license, a person must answer questions if
they have any physical or mental conditions that could impair their driving skills
or cause loss of consciousness or control. They also must certify their answers by
signing the document.
If a Montana driver responds yes to one of the questions, MVD may require them to
have their primary physician complete a Driver Medical Evaluation, Form 20-1900, https://dojmt.gov/wp-content/uploads/mv20-1900.pdf. The results of the medical evaluation will determine whether the person needs further
testing, such as taking a driving and/or written test.

Photo: Shelley Mills
If a physician completes a medical evaluation form with negative results, MVD will
not issue a driver’s license to the person. In addition, at the time of licensing,
if an examiner sees or has evidence that a driver may not be safe to drive a motor
vehicle, MVD may require a driving and written test separate from a medical professional’s
evaluation. Further information is available from the Motor Vehicle Division, Driver
Services Bureau. Call 406-444-1772 or visit the website, https://cars.dojmt.gov/app/_/#1.
Driving with firearms in the vehicle
Montana farmers and ranchers occasionally travel with a rifle in a vehicle. If Alzheimer’s
is suspected or if a physician has diagnosed it, the rifle and ammunition, plus any
other firearms, should be removed from the vehicle. This is for the safety of everyone.
Limitations on driving
Because the progression of Alzheimer’s varies from person to person, some farmers
or ranchers who drive safely in the early stage of Alzheimer’s disease may need to
gradually decrease driving. This can reduce the risk of accidents if their driving
skills decrease significantly between licensing years. Making the transition from
driver to passenger over time can help ease the adjustment. Encourage the person to
avoid:
- Unfamiliar roads
- Driving long distances
- Heavy traffic and heavily traveled roads
- Driving at night
- Driving in severe weather
- Driving with an unlicensed adult
Involve the farmer or rancher in discussions about driving
Some people with early signs of Alzheimer’s are aware of their driving challenges
and decide on their own to quit driving. A few are relieved when family members encourage
them to stop driving. Others find the loss of driving privileges and independence
to be confusing, disturbing, distressing, and frightening. They may refuse to stop
driving, even after the state has revoked their license.
Consider who is most likely to have ‘listening leverage’ with the person about driving.
The farmer or rancher may be more receptive to suggestions from another family member,
good friend, or doctor instead of the caregiver. During a discussion about driving,
the farmer or rancher may ask questions to justify their continuing to drive:
- How will the wheat get harvested if I don’t drive the combine?
- How will the hay get baled if I don’t run the swather?
- How will the crops get planted and shipped if I can’t drive the tractor or truck?
Try to imagine what it would be like to no longer drive. Think about the places you
drive, people you visit, and your activities requiring a vehicle. This will help bring
empathy and awareness of the person’s feelings and concerns.
Communicating with a farmer or rancher about driving concerns is not an easy conversation.
Losing the ability to drive is difficult and frustrating for the individual. People
often adjust better when they take part in discussions about reducing and eventually
stopping driving. The approach to discussing this with a person with Alzheimer’s is
critical. Making accusations of unsafe driving has little chance of success and is
likely to provoke anger, denial, and defensiveness.
When communicating with the farmer or rancher, show empathy and acknowledge how difficult
the decision is to reduce or stop driving. Try to be compassionate and caring. Be
sensitive to both the symbolic meaning and practical significance of driving. Acknowledge
hearing their thoughts and feelings to enhance communication. Show respect and admiration
to the person who makes a responsible decision.
Balancing safety with respect for a farmer or rancher’s desire to drive can be difficult
and emotionally trying for everyone. When a person can no longer drive, depression
is common. Enlist the support of family members, friends, and health professionals
to recognize depression and acknowledge the person’s feelings of loss. Support groups
can be helpful for both the family caregiver and the person with Alzheimer’s. Talking
about feelings and getting ideas from others in similar situations can be beneficial.
Some people with Alzheimer’s are not able to recognize their impairment or limitations.
They may overestimate their driving ability. This is because their brain has been
compromised, not because they are purposely being difficult.
Begin discussions early and set guidelines about when and how to limit and eventually
stop driving. Try to reach an agreement with the farmer or rancher about driving behavior
that signals the need to stop driving. Each family will need a solution that works
best for their situation.
Include a physician, attorney, or law enforcement officer in the discussion
If the farmer or rancher is reluctant to talk about driving, consider asking the individual’s
physician to discuss the subject of health and driving during the next appointment.
For some people, a doctor’s advice is the most influential.
An attorney may also be willing to discuss driving as part of a legal checkup. The
attorney could share about the possibility of a lawsuit and losing the farm or ranch
if an accident results in the injury or death of another person.
A family member may request a local law enforcement officer to come to the home to
ask the person who has Alzheimer’s to relinquish the keys. This may be a useful approach
if the person is unwilling to part with the keys without direct authority.
Individuals with moderate or severe Alzheimer’s should not drive.
Selling the vehicle
All too often when a farmer or rancher must give up driving, family and friends think
it’s best to remove the temptation to drive by selling a vehicle. However, because
of a vehicle’s symbolic meaning of independence, keeping it may be important, even
if it is never driven. A farmer or rancher may feel less dependent if they can offer
their vehicle for use when they depend on others for transportation.
Arrange for alternative transportation
Make a list of activities the person wants to do that require transportation. Then,
arrange for rides to support the person’s mobility and activities. Ask family members,
friends, and neighbors if they are willing to drive the farmer or rancher to social
engagements and appointments. Record their names, telephone numbers, and availability
in an address book.
Some Montana counties have volunteers at senior centers, an Area Agency on Aging,
community groups, and churches who will drive older adults to activities and appointments.
Are there any organizations in the community that offer transportation? Could a neighbor
start a rural taxi ride service?
Summary
Caregivers, friends and family of a person with Alzheimer’s can help with safe driving
decisions and ease the transition to giving up driving. Signs of unsafe driving should
alert family members to discuss safe driving or to take away the keys. Setting up
a schedule for rides becomes a must.
Signs of Unsafe Driving
The Family Caregiver Alliance has suggested guidelines to help families and individuals
with Alzheimer’s decide when and how to limit or stop driving, www.caregiver.org/resource/dementia-driving.
The following may be warning signs that a person’s driving threatens the safety of
self and others. When any of these signs are seen, it is time to assess the situation
and take necessary precautions.
ATTENTION/CHANGE IN HABITS
- Does not notice or pay attention to traffic signs
- Does not see pedestrians, objects, or other vehicles
- Does not pay attention to road hazard signs
- Does not follow traffic laws, road signs or signals
- Makes slow or poor decisions in traffic, stops for no reason
- Confuses brake and gas pedals
- Hits curbs
- Signals incorrectly or forgets to use turn signals
- Drives significantly faster or slower than the posted speed limit or traffic flow
- Gets drowsy or falls asleep while driving
- Becomes angry, confused, increasingly nervous, or irritated while driving
- Gets tickets for traffic violations
- Gets into minor accidents (look for dents or scratches on the vehicle)
TRIP DESTINATION DIFFICULTIES
- Returns from routine drives later than usual
- Forgets the trip destination when driving
- Becomes lost on familiar routes
- Forgets where they have been
- Cannot find the way home
TRAFFIC LANES
- Drifts into other lanes or makes poor lane transitions
- Makes errors at intersections, such as not yielding right-of-way
- Has difficulty with turns, lane changes, or highway exits
- Weaves in and out of traffic too close to other vehicles
- Drives on the wrong side of the road
- Parks inappropriately over parking lines and uses two spaces
Wandering: A Safety Concern
SIX OUT OF 10 INDIVIDUALS LIVING WITH ALZHEIMER’S wander at least once; most will wander repeatedly. Wandering is dangerous, especially
for individuals living and working in an agricultural environment. Many farms and
ranches in Montana consist of hundreds or thousands of acres and open spaces.
Farmers and ranchers with Alzheimer’s may become disoriented on their own property.
They may get lost in a community where they have lived for years. They also may wander
when traveling with other people. A farmer or rancher may respond with “OK” to a request
to “stay right here” while others go elsewhere, but then does not remember what was
said and wanders away. They may start searching for someone they know or a familiar
landmark and become lost.
Wanderers may not know when they are lost. They may:
- not remember the location of their home on their farm or ranch property.
- face sudden rain or snowstorms and not be dressed appropriately for the weather.
- come across bodies of water deeper than they realize.
- pass out from exhaustion.
- not know how to use their cell phone and be unable to make a call for help.
Plan ahead
The stress experienced by families and caregivers when a farmer or rancher living
with Alzheimer’s wanders and becomes lost is significant. With a plan in place, everyone
will know what to do if a person wanders.
- Consider enrolling the person in the Alzheimer’s Association’s nationwide 24/7 Wandering Support for Safe Return Service, www.alz.org/documents/national/card_wanderingwhoisatrisk.pdf.
- Ask neighbors, friends, family, and local retailers to call if they see the farmer or rancher wandering, appearing lost, dressed inappropriately for the weather, or alone in an unusual or dangerous area.
- Family members should notify local law enforcement that the farmer or rancher has Alzheimer’s and may wander.
- Keep a recent, close-up photo of the person with Alzheimer’s to give to the local sheriff in case a photo is needed for identification.
- Identify potentially dangerous areas on the farm or ranch and nearby, such as bodies of water, cliffs, dense foliage, or roads with heavy or fast traffic.
Reasons a person may wander
Wandering can occur due to various circumstances, including stress, overstimulation,
confusion, medication, fear, or the person’s inability to recognize their surroundings.
Wandering behavior may stem from a farmer’s or rancher’s need to move. If true, take
them on frequent walks or offer other physical activities such as raking leaves or
shoveling snow from the porch or driveway. Regular exercise may also relieve tension
and improve a person’s sleep.
To prevent and reduce wandering, ask yourself, “What are possible reasons the person wanders?”
- Did the farmer or rancher previously enjoy walking the property and doing other outdoor
activities?
- Did the person often walk to reduce stress?
- Is the farmer or rancher bored?
- Is there a place the person wants to go?
- Is the person looking for someone or something related to their past?
- Was the person trying to get away from someone?
- Was the person trying to avoid an unfamiliar or uncomfortable situation?
- Did something on television frighten or upset them?
- Did an unusual noise attract their attention, such as a fire truck with sirens driving by or road construction near the house?
- Was the person overstimulated or overwhelmed by an activity, too many people, or too much noise?
- Did the environment change on the farm or ranch?
- Is the person in an unfamiliar location?
- Does the person recognize their current home as “home,” or do they leave to find their “home?”
- Is the person trying to fulfill former obligations, such as going to town to work at a local business they ran years ago?
- Is the person searching for a sense of security, for example when they say, “I want to go home” or “Where is my mother?”
- Is the wandering because the farmer or rancher thinks it’s time to perform a task? For example, the person may believe, “It’s time to feed the hogs, chickens, horses or sheep.”
Track the person’s wandering behavior to see if there is a pattern. Is there a time of day when wandering occurs most often? Wandering may have no specific cause other than being a symptom of Alzheimer’s.

Photo: Adobe Stock
Reduce the risk of wandering
The Alzheimer’s Association offers the following tips to reduce the risk of wandering.
Being prepared can bring family members peace of mind. However, these actions cannot
guarantee a person living with Alzheimer’s will not wander.
- Offer opportunities for the farmer or rancher to engage in structured, meaningful activities throughout the day.
- Identify the time of day when the person is most likely to wander such as late afternoon or early evening as daylight wanes. Plan things to do during this time. Activities and exercise may help reduce anxiety, agitation, and restlessness.
- Consult with their doctor about reducing – but not eliminating – liquids up to two hours before bedtime so the person is less likely to have to find and use the bathroom during the night.
- Involve the person in daily activities with another family member or farm or ranch hand to help check the fencing for damage or see if pests are affecting the crop.
- Provide reassurance if the person is agitated, lost, or disoriented.
- Avoid busy places that create confusion or disorientation and cause the person to be overstimulated such as trade shows, conferences, shopping malls, local fairs, grocery stores, or holiday celebrations.
- Assess the person’s response to new surroundings that may cause confusion, uncertainty, or agitation.
- Never leave a farmer or rancher with Alzheimer’s alone in a parked vehicle with the keys left inside. They could cause an accident by starting the vehicle and driving away. Or they could leave the vehicle and wander.
- Review medications with their doctor to learn if one or more may be causing confusion and delusions.
When someone with Alzheimer’s goes missing, begin search-and-rescue efforts at once.
According to the Alzheimer’s Assocation, many individuals who wander are found within
1.5 miles of where they disappeared.
Most cell phones have a GPS feature that can track a family member’s location. Consider
attaching a small GPS-guided tracking device to the person’s clothing and using an
app to track the GPS unit. Recommendations about tracking devices are available online,
www.medicalalertbuyersguide.org/articles/the-best-gps-trackers-for-dementia-patients.
Have the farmer or rancher always wear an identification or medical-alert bracelet
showing their name, address, telephone number, and the phrase “memory-impaired” or
“brain-impaired.” Unfortunately, listing the official diagnosis, such as “Alzheimer’s”
or “dementia,” may not be helpful because some people who see a wanderer may not know
the meaning of the words.
Approaching a family member or neighborhood wanderer who has Alzheimer’s
Approach a wanderer slowly and calmly from the front. Offer reassurance. Gently ask,
“May I walk with you for a while?” Walk a short distance in the same direction they
are going, and then, gradually turn them in the direction of home.
Another strategy is to redirect the wanderer to an activity they enjoy. For example,
say, “I have your favorite cookies and ice cream back at the house.” or “Your favorite
TV program is on soon.”
Do not hurry, scold, restrain or use physical force. Such actions usually make a person
more agitated, confused, and angry. Do not expect the person to understand the reasoning
and logic for returning to their home.
Summary
During the middle to late stages of Alzheimer’s, people begin to lose their ability
to recognize familiar places. They may wander in search of their home. When a person
wanders and becomes lost, both the wanderer and the family experience stress. Make
early plans about what to do if a family member with Alzheimer’s wanders.
Safety Measures in the Home and Surrounding Environment
WHEN FAMILY MEMBERS SUSPECT A FARMER OR rancher has Alzheimer’s or if a physician has diagnosed it, a long-term strategy needs
to be developed for the person’s safety. Risks can range from working with temperamental
livestock to operating large machinery such as tractors and combines, grain bins,
and other equipment. Even the location and landscape of the farm or ranch may present
safety risks.
One rancher said he believes controlling access to keys is the most important safety
measure because it’s common to leave keys in trucks, ATVs, tractors, and combines.
Access to keys makes it possible for a person with Alzheimer’s to start a vehicle,
drive off, and get lost, an incident that occurred in his community.
As Alzheimer’s progresses, adjustments will need to be made in the farmer’s or rancher’s
role. This can be a gradual process, such as doing more repetitive tasks in a controlled
environment. Work tasks and chores that can be done by the farmer or rancher while
working with others can be suggested. Involve family members or hire a farm or ranch
hand to provide some relief.
Doing simple, safe tasks can lead to feelings of worth and purpose for someone with
Alzheimer’s. Gathering eggs, filling and emptying feed buckets, and grooming horses
could all be included in the daily routine. Maintaining equipment such as greasing
parts, cleaning the cab of tractors and combines, and sweeping the shop are also productive
and relatively safe.
Taking steps to increase safety in the home and on the farm and ranch benefits both
the person with Alzheimer’s and the family caregiver. This article covers a broad
range of safety concerns that may arise. While some modifications discussed may never
be needed, re-evaluating the safety of the environment is important because the person’s
abilities and behavior will change as Alzheimer’s progresses.

Photo: Adobe Stock
General safety measures to consider for all rooms in the home include:
- Remove items in each room a person could trip over, such as rugs, footstools, and electrical cords.
- Cover electrical outlets.
- Install childproof door latches on storage cabinets and drawers used for breakable and dangerous items (e.g. hazardous sprays and insecticides).
- Secure the family junk drawer. A person who has Alzheimer’s may eat small items such as matches, erasers, watch or hearing aid batteries, and plastics found in the drawer.
- Remove toxic plants and decorative fruits that could be mistaken for real food.
- Secure large furniture, such as bookshelves, cabinets, and televisions to prevent tipping.
- Make sure chairs have armrests to provide support when the person moves from a sitting to a standing position.
- Remove guns and other weapons from the home or store them in a locked cabinet or gun safe. As the disease progresses, people may not recognize someone they have known for years and view them as an intruder.
- Print simple safety signs in a large font, such as STOP, HOT, or WATCH YOUR STEP, to remind people to pay attention.
- Make memory aids such as labels to place on appliances and drawers in the kitchen, shop, bathroom, nand bedroom.
- Replace word labels with pictures when the person no longer understands the written word.
- Place red tape around floor vents, radiators, and other heating devices to discourage the person who has Alzheimer’s from standing on or touching them when hot.
- Be prepared for a crisis by keeping a list of emergency telephone numbers and addresses for local police, fire department, hospital, and poison control helplines.
- Keep fish tanks out of reach. The combination of glass, water, electrical pumps, and potentially poisonous aquatic life could harm a curious person with Alzheimer’s.
Bathroom
- Install grab bars next to the toilet and where there are slick surfaces such as the
bathtub or shower.
Photo: Adobe Stock
- Add a chair to the shower or install a transfer bench to the bathtub.
- Use a rubber mat or no-skid stickers on the bottom of the bathtub and shower to prevent falls.
- Use a foam rubber faucet cover (often used for small children) in the bathtub to prevent severe injury should the person fall.
- Install a heat-resistant cover if the bathroom has an electric heater.
- Adjust the house water temperature to 120 degrees. For an added layer of protection, consider installing an anti-scald, pressure-balancing valve.
- Install night lights in the bedroom, hallway, and bathroom.
- Remove small electrical appliances. If a man or woman with Alzheimer’s uses an electric razor, hair dryer, or curling iron, ask them to use a mirror outside the bathroom to avoid dropping the appliance in a sink of water.
- Cover mirrors if the person is in a later stage of Alzheimer’s and no longer recognizes themself. They may believe the person in the mirror is a stranger in their home.
Bedroom
- Place a strip of glow-in-the-dark tape from the bedroom to the bathroom. This light
trail
increases nighttime safety and helps orient the person.Awakening in the dark can be disorienting to a person with Alzheimer’s, and they may become frightened and upset.
Photo: Adobe Stock
- Check an electric blanket and/or heating pad for any loose wires to prevent shock and electrical burns.
- Provide a place to sit near the bed to help with dressing and undressing.
- Make sure closet shelves are at an accessible height so items are easy to reach. This may prevent the person from tipping shelves forward or having objects fall on them.
- Place a pressure-sensitive mat on the floor beside the bed to alert the caregiver to the person’s movements. Be sure the sound alert is in the caregiver’s room and not in the room of the person with Alzheimer’s. A loud noise in the middle of the night could frighten them.
Kitchen
- Remove knobs from the range to prevent a person from turning on the gas or electric range and forgetting to turn it off.
- Disconnect the garbage disposal because a person may place objects or their hands in it.
- Remove vitamins, prescription drugs, sugar substitutes, and seasonings from the kitchen table and counters.
- Look in the oven and microwave before turning them on because a person who has Alzheimer’s may have placed flammable materials or items that will melt in either one or both.
- Keep plastic bags out of reach because a person may no longer understand the danger of suffocation.
Laundry room
- Keep all cleaning products – such as liquid laundry packets and bleach – out of sight, secured and in the original (not decorative) storage containers to discourage the person from eating or touching harmful chemicals.
Stairs
- Place a gate across the top of the stairs to prevent a fall.
- Install handrails on both sides of the stairs so the person is more safe going up and down.
- Have at least one handrail extending beyond the first and last steps of stairs to help with balance.
- Install carpets or a non-slip tread on stairs.
Doors inside and outside
- Remove locks on bedroom and bathroom doors to avoid accidental locking.
- Place a pressure-sensitive mat in front of doors leading outside to alert the caregiver when the person is at the door.
- Install a warning alarm on doors or use a monitoring device that signals when the person opens a door to the outside.
- Consider installing door locks either high or low on exterior doors, out of a person’s line of sight. NOTE: Always ensure an emergency exit is available.
- Store items out of sight that are likely to prompt a person to want to leave the house. These include coats, hats, purses, billfolds, gloves, suitcases, and keys.
- Use black tape, paint a piece of cardboard, or use a black floor mat to create a two-foot black threshold in front of exterior doors to function as a visual stop barrier. It may be perceived as a hole and discourage the person from opening the door.
- Camouflage the inside of exterior doors by painting them the same color as the walls; cover doors with removable curtains, quilts, or screens; or add posters that make doors look like something else, such as a bookshelf.
Medication and dangerous substances
- Be sure the person takes medications exactly as prescribed.
- Store medicine bottles out of sight and/or in a locked container to prevent the person from taking medications on their own.
- Lock potentially dangerous items, such as firearms, power tools, small appliances, knives, scissors, razor blades, poisons, and cleaning supplies.
Safety devices
- Install carbon monoxide and smoke detectors.
- Replace batteries in detectors at least twice a year.
- Know the location of the fire extinguisher and have it inspected regularly.
Garage and basement
- Limit access to power equipment stored in the garage such as lawnmowers, weed trimmers, and snow blowers.
- Keep poisonous chemicals such as gasoline and paint thinner out of reach or in a locked cabinet.
- Install a motion sensor light on the garage door to increase the visibility of the driveway and surrounding area.
Fall prevention
- Move the family dog or cat to another area if they jump on people or walk between their legs. This pet behavior adds to the risk that the person may lose their balance, trip, and fall.
- Make arrangements with 911 providers to help in case a person falls and cannot get up. Explain that when emergency help is requested to come without sirens because the sound could scare or agitate the farmer or rancher.
- Use a monitoring device (like those used for infants) to alert the caregiver to any noises that sound like a fall or a shout for help. This can also be an effective device for bathrooms.
- Prevent the person from going outside when the sidewalks and driveway are icy. If
they refuse, be sure they wear boots with traction and use a walking aid.
Other Resources About Safety (specific to the home)
Vicki Schmall, Emerita Professor and Extension Gerontology Specialist, Oregon State
University and colleagues published Helping Memory-impaired Elders: A Guide for Caregivers,
which has suggestions for protecting the person in the home. http://extension.oregonstate.edu/catalog/pub/pnw-314-helping-memory-impaired-elders-guide-caregivers
The National Institutes of Health has a “Home Safety Checklist for Alzheimer’s Disease.”
https://www.nia.nih.gov/health/safety/alzheimers-caregiving-home-safety-tips
The Alzheimer’s Caregiver’s Network has a room-by-room checklist. https://alzheimerscaregivers.org/2023/02/07/home-safety-alzheimers-disease-a-caregivers-room-by-room-checklist/
Outside the home (barns, corrals, livestock facilities)

Photo: Adobe Stock
- Make sure outdoor lighting is adequate. Motion sensors that turn on lights automatically as the person approaches the house from the driveway, barn, or corral may be beneficial. Motion sensor lights may also be helpful in other parts of the home, garage, or basement.
- When not in use, remove any fuel sources and fire starters from the grill in the patio area or deck.
- Supervise a person who has Alzheimer’s when they are using the grill.
- Keep walkways or paths clear of rocks, roots, sticks and other debris to prevent tripping or falling.
- Check outdoor areas such as yards and gardens regularly for poisonous plants and mushrooms during the growing season.
- Make grain bins and hay and feed storage areas inaccessible, whether full or empty.
- Lock up garden tools such as rakes, pruning shears, handsaws, shovels, hoes, and other similar tools.
- Provide supervision when the person uses a lawnmower, rototiller, or weed eater.
- Lock cabinet doors to prevent access to hazardous items such as pesticides, herbicides, fungicides, fertilizers, veterinary chemicals, and flammable liquids.
Comments about safety from Montana farmers and ranchers and their families
In researching information for this article, several Montana farmers, ranchers, and
family members were asked to share thoughts about memory loss and safety. What follows
is a summary of their observations.
- While all animals pose a risk, some are more dangerous than others. Mother cows, when calving, pose a unique risk to a person with Alzheimer’s who no longer has the intuition to read the animal and move accordingly. Bulls, while docile in the winter, become large locomotives when spring arrives. Even if they aren’t mean, their vast size creates a hazard when they are determined to go somewhere or are wrestling with other bulls. Horses, sheep, and pigs, while smaller in size, also pose a risk because someone with memory loss may not be able to respond to unexpected animal behavior.
- In my mind, the biggest challenge is having enough help to cover all the tasks that the farmer or rancher can no longer safely perform.
- I think it is important to go through every inch of the farm or ranch to make sure all tools and equipment are in a safe place and that ATV and pickup truck keys are removed.
- I feel like people in agriculture have a very independent nature that borders on stubbornness which could lead to unsafe decisions.
- Ladders, chain saws and other tools pose problems when they are easily accessible.
Lock them up. My husband was always climbing ladders to look in
the grain bin or mess with something on the roof of the house. - One problem with a rural lifestyle is the distance to get groceries, daily necessities, and medical help. There is no delivery in rural places, and even getting 911 help may not be practical.
- Another common part of rural living is traditional role expectations. In our family, men do the outside work and rely on women to provide meals and run to town for parts and supplies. Each role has its own safety concerns.
- If one is capable of operating farm and ranch equipment, care must be taken to make sure the equipment is in good working order. The machinery sounds that used to be obvious and suggest a problem may not be interpreted as such by a person with Alzheimer’s.
- Irrigation is a unique danger. Flood irrigation involves canals and ditches full of water, slippery mud and the risk of falls and drowning. Sprinkler irrigation means moving parts and precise settings which could be altered by someone with memory loss, causing breakdowns.
- Block access to stairs and ladders going up to the hay loft in barns or upper levels in buildings.
- Store implements in a secure location. These could be simple tools such as rakes and shovels or more dangerous tools such as pitchforks, axes, and ice chippers.
- Locking gates or doors should restrict access to barns, corrals, pastures, and other livestock facilities used for housing animals. This includes all livestock: cattle, horses, sheep, pigs, poultry, and other livestock production animals.
Summary
Behavioral and cognitive changes in people with Alzheimer’s often make it difficult
for them to remain safe in their homes and surroundings. They may forget
how to use appliances and tools and no longer recognize hazards or changes in familiar
surroundings. They may wander and become disoriented or confused when leaving the
house. A farmer or rancher may not remember to follow safety instructions when operating
equipment.
Dung Trinh, MD, owner and founder of Healthy Brain Clinic, said people with Alzheimer’s
disease may also experience changes in their balance and coordination, which can increase
their risk of falls, especially when walking around fields, corrals, and roads.
“Taking steps to make the home environment safe is an important part of managing Alzheimer’s
disease,” said Trinh. “A thorough area-by-area safety check can help identify areas
where additional safety measures may be needed.”

Photo: Katie Hatlelid
Planning for the Cost of Long-Term Care
LONG-TERM CARE EXPENSES are the largest out-of-pocket health care expense for older adults, including farmers
and ranchers. Costs vary by location. In 2024, monthly median costs for a semi-private
room in a nursing home range from $4,483 in Texas to $19,267 in Alaska. Below are
the 2023 average costs for the five types of long-term care in Montana.
Average Cost of Long-Term Care in Montana (2023)
| Monthly | Yearly | |
|---|---|---|
| Homeaker Services | $9,483 | $113,256 |
| Home Health Aide | $6,673 | $80,800 |
| Adult Day Health Services | $3,445 | $41,340 |
| Assisted Living Facility | $4,908 | $58,890 |
| Nursing Home Facilty | ||
| Semi-Private Room | $8,182 | $98,185 |
| Private Room | $8,465 | $101,470 |
Source: 2023 Genworth Cost of Care Survey.
www.genworth.com/aging-and-you/finances/cost-of-care
Some farmers and ranchers mistakenly believe Medicare pays for long-term care. Medicare
and most other health insurance, including Medicare Supplement Insurance (Medigap)
plans do not pay for non-medical long-term care. Medicare only pays for skilled services
or rehabilitation if prescribed by a physician. Medicare Part A does cover skilled
care services in a nursing home for up to 100 days per benefit period if a person
meets all of the conditions listed at medicare.gov/coverage/skilled-nursing-facility-care.
Medicare also pays for services at home if the person needs home health or other in-home
skilled services. More information about Medicare is available online at https://www.medicare.gov/coverage/skilled-nursing-facility-care. Medicare also pays for services at home if the person needs home health or other
in-home skilled services. More information about Medicare is available online at https://www.medicare.gov/coverage/long-term-care.
Who will need long-term care?
The Administration on Aging, a part of the U.S. Department of Health and Human Services,
reports:
- People age 65 and older have a 67 percent chance of needing long-term care.
- Approximately 70 percent of people aged 65 and older will require long-term care services at some time in their lives.
- The average woman needs long-term care services for 3.7 years, while an average man needs those services for 2.2 years.
- A person with Alzheimer’s or other forms of dementia may need long-term care longer.
- While one-third of people aged 65 and older may never need long-term care, 20 percent will need it for longer than five years.
Long-term care services
A person with Alzheimer’s will need more advanced care (typically referred to as long-term
care) as the disease progresses. Many people automatically think of care in a nursing
home, but long-term care also includes home-based care services, adult foster care,
assisted living facilities, residential care, memory care, and skilled care facilities.
According to the Alzheimer’s Association, individuals and their families often pay
out-of-pocket for respite, home health, and nursing home care. In some Montana communities,
adult day care and senior center programs – for example, on-site lunches, home-delivered
meals, exercise programs, social activities, and transportation – are available at
no cost or for a fee.
Skilled nursing is typically provided for a limited period, often following a hospital
stay, to help patients who are recovering from an illness or injury. The goal
is to help patients regain their physical abilities and self-sufficiency so they can
return to their normal daily activities. The Montana Health Care Association has a
list of the state’s licensed skilled nursing facilities. http://www.montanahealthcareassociation.org/skilled-nursing-facilities.html.
Memory care is also provided at long-term facilities in the state. These facilities
are licensed and provide services to individuals in a controlled environment. According
to the Montana Department of Public Health and Human Services, there are 63 long-term
care facilities in Montana offering personal care, social and recreational activities,
meals, and medical services.
During 2024, the average daily cost for a semi-private room in Montana nursing facilities
is $286.71, or $8,601.30 monthly, or $104,649 yearly. Given the high cost of long-term
care, it’s no wonder farm and ranch families would ask themselves:
“How are we going to cover the potential cost of long-term care without losing what
we have worked so hard to accumulate as a legacy for our families?”
Sources to pay for long-term care
Montana farmers and ranchers can use various sources to pay for long-term care, including personal income and savings, annuities, Medicaid, long-term care insurance, long-term care partnership insurance, a reverse mortgage, Veterans benefits, and/or family financial support.
PERSONAL INCOME AND SAVINGS
Some Montana farm and ranch families plan to pay for the cost of long-term care from their present income, savings, investments, IRAs, or other retirement plans.
Others expect to borrow from their life insurance policies. Unfortunately, some face
selling their home, farm or ranch to fund needed long-term care.
A farmer or rancher paying with their own funds can select a private room in a care
facility. With Medicaid, they would have fewer choices because long-term care facilities
can limit the number of publicly funded residents and place two people in each room.
ANNUITY

Photo: Anna Dupus
Another way for farmers and ranchers to pay for the cost of long-term care is to buy
an annuity. An annuity is a written contract, typically between a person and a life
insurance company. The life insurance company makes a series of regular payments (monthly,
quarterly, or annually) to the “annuitant” in return for premiums paid. A farmer or
rancher can use annuity payments for any type of long-term care.
The primary advantage of an annuity is that the farmer or rancher makes payments to
the company over time. Another benefit is that the company guarantees regular payments.
However, all commercial and private annuities, including single premium life endowment
policies, should be examined to see if they must be assigned to Montana Medicaid prior
to eligibility determination. Annuity ownership, accessibility and equity value should
also be assessed.
Drawbacks of an annuity are charges for agent commissions, annual maintenance fees,
and penalties if an annuitant withdraws the funds early. More information is provided
in the MSU Extension MontGuide Annuities, https://store.msuextension.org/Products/Annuities-MT199213HR__MT199213HR.aspx.
MEDICAID
This public insurance program provides health coverage to low-income families and
individuals, including children, parents, pregnant women, older adults, and people
with disabilities. The program is funded jointly by federal and state governments.
A farmer or rancher who applies for Medicaid must meet the assets and income tests
for eligibility. Assets must be less than $2,000, and income must be less than the
cost of long-term care. The application process for Medicaid includes completing three
forms: a pre-screening medical determination, a resource assessment, and an application
for assistance.
The Aging and Disability Resources Center (ADRC) in Montana can help farmers and ranchers
find local Medicaid providers and other Medicaid resources in their community, including
licensed nursing homes, in-home care providers and other forms of long-term care.
The ADRC offers help with long-term care planning through its Montana Options Counseling
service, https://dphhs.mt.gov/SLTC/aging/adrc/.
Making gifts to qualify for Medicaid. Some farmers and ranchers believe the best protection
against depleting their assets for long-term care is to become impoverished. They
believe if they give away all their property they will automatically qualify for Medicaid.
This is NOT correct!
Look-back period for Medicaid. Medicaid has a period of ineligibility if an applicant
gifts an asset to others during the look-back period. Any asset transfer made by the
applicant has a look-back period of five years before their Medicaid application date.
Giving away the house, farm, or ranch to adult children is not a solution.

Photo: Jane Wolery
The amount of time an applicant is ineligible for Medicaid depends on the value of
a gift and when it was made. The period of ineligibility is calculated by taking the
value of the gifted assets and dividing it by the daily cost of a room in a long-term
facility. For fiscal year 2024, Montana’s semi-private average daily cost of nursing
home care is $286.71. The period of ineligibility is one day for every $287 (rounded)
in value of assets the applicant gave away.
Example: John gifted stocks from the ranch corporation valued at $195,000 to his grandchildren,
adult children, and their spouses. If John applies for Medicaid within five years
of making his gifts, they are subject to the five-year look-back rule. John has almost
two years of ineligibility for Medicaid ($195,000 amount of his gifts ÷ $287 daily
cost of nursing home care = 679 days ÷ 365 days in a year = 1.86 years). Would John’s
grandchildren, adult children, and their spouses come forward with the gifted money
to pay for his care for almost two years?
Because financial gifts can have legal, emotional, and tax consequences, a farmer
or rancher should discuss their financial situation with an accountant and attorney
before making such gifts. For more information, download the MSU Extension MontGuide
Medicaid and Long-Term Care Costs, https://store.msuextension.org/publications/FamilyFinancialManagement/MT199511HR.pdf.
Medicaid and Medicare Counseling.
The State Health Insurance Assistance Program (SHIP) is offered in Montana. SHIP provides one-on-one counseling about Medicaid, Medicare, and Medicare Supplemental Insurance (Medigap) plans. A SHIP counselor can help farmers, ranchers, and their caregivers navigate Medicaid eligibility, coverage, appeals, and out-of-pocket costs. Learn more about SHIP online at https://dphhs.mt.gov/sltc/aging/ship, or call 1-800-551-3191.
LONG-TERM CARE INSURANCE
Long-term care insurance provides protection against significant expenses associated with a prolonged illness, such as a person with Alzheimer’s needing extended care. Answering the following questions can help a person make a decision about buying long-term care insurance:
- How much will the policy pay per day? Is the rate indexed for inflation, and if so, how is the indexing calculated?
- When does payment coverage begin? On day 1, day 30, day 100?
- Does the policy have a maximum lifetime benefit? If so, what is the amount?
- Are optional benefits available under the policy, and if so, what is the cost?
Before buying long-term care insurance, the Montana Department of Public Health and Human Services recommends considering these factors:
- premium costs
- length of time the company has been writing this type of insurance
- the insurance company’s payout history
- company’s history of premium increases
- specific type of services covered under the policy
- number of years the policy will pay benefits
- company policy towards pre-existing conditions
- conditions under which the company may waive premiums
The National Association of Insurance Commissioners (NAIC) has a resource guide, A Shopper’s Guide to Long-term Care Insurance, which can be downloaded or ordered without charge at https://csimt.gov/wp-content/uploads/2022/10/publication-ltc-lp-shoppers-guide-long-term.pdf. The Shopper’s Guide suggests:
- Carefully compare policies under consideration, as they are NOT all the same.
- Check with several agents and companies before making a purchase.
- Be sure the agent provides an outline of coverage at the time of agent contact, as this is a requirement under Montana law.
- Do not let an agent apply pressure to make a quick decision.
- Invite the agent back for a follow-up visit. Tell the agent a trusted friend or family member will be reviewing the policy information before the purchase.
- Never pay the agent with cash. Write a check or use a credit or debit card and get a receipt of payment.
- Be sure to have a written record of the name, address, and telephone number of both the agent and the company represented, in addition to policy details.
- Take advantage of a 30-day “free-look” period if buying a policy. Be sure to thoroughly review the policy details to make sure the policy covers what was intended.
LONG-TERM CARE PARTNERSHIP INSURANCE PROGRAM
The purpose of the long-term care partnership insurance program is to provide an incentive
to Montanans to buy long-term care insurance partnership policies. This will reduce
the amount of money spent by the state for long-term care under the Medicaid program.
Also, the program provides some protection for Montanans from having to spend down
their resources to qualify for Medicaid benefits.
When a Montanan who bought a qualified long-term care partnership insurance policy
needs care, the benefits will help cover costs of care up to the policy’s lifetime
benefit limit (often called benefit pool). If a person reaches the lifetime limit
and still needs long-term care, any assets equal to the value of the policy limit
are not included if a person applies for Medicaid.
Example: Betty Lou is a farm widow who bought a long-term care partnership insurance policy
when she was age 55. The lifetime benefit pool for Betty Lou’s policy was $100,000.
By age 72, Betty Lou’s remaining assets included $2,000 in her checking account and
$75,000 in certificates of deposit (CDs) she wanted to leave to her two grandchildren.
When Betty Lou needed long-term care because of Alzheimer’s, first in her home and
later in a nursing home, the benefits of the partnership policy covered her expenses
until the lifetime pool of $100,000 was reached. When Betty Lou became responsible
for payments to the nursing home, her daughter visited the local Office of Public
Assistance (OPA) and showed documentation from the insurance company of Betty Lou’s
use of the lifetime benefit pool of $100,000 from her qualified long-term care partnership
insurance policy.
Betty Lou was able to keep the CDs ($75,000) to leave to her grandchildren and the
$2,000 in her checking account because she had bought and used the $100,000 benefit
pool of her qualified long-term care partnership insurance policy. Betty Lou did not
have to spend down her remaining resources of $75,000 before becoming eligible for
Medicaid. Betty Lou could have kept up to $100,000 of her assets because $100,000
was the benefit pool amount.
The website of the Montana Commissioner of Securities and Insurance provides links to 19 companies in Montana selling long-term care partnership policies, https://csimt.gov/your-insurance/long-term-care/.
More information is available in an MSU Extension MontGuide, Long-Term Care Partnership Insurance in Montana, https://store.msuextension.org/Products/Long-Term-Care-Partnership-Insurance-in-Montana-MT201202HR__MT201202HR.aspx
REVERSE ANNUITY MORTGAGE PROGRAM
A reverse annuity mortgage is a special type of home equity loan that allows a person
to receive cash against the value of a home without selling it. The home must be in
Montana. Mobile and manufactured homes are not eligible. The Department of Commerce
oversees the program.
A farmer or rancher can choose to receive a lump-sum payment, a monthly payment, or
a line of credit. There are no restrictions on how the money is spent. A person can
continue to live in their home and keep the title and ownership. The owner continues
to pay property taxes, homeowner’s insurance, and home repairs.
If a farmer or rancher continues to live in their home while receiving long-term care
services, they typically do not have a traditional loan repayment. Instead, the amount
they owe, based on loan payouts and interest on the loan, becomes due when the farmer
or rancher or the last borrower, usually the surviving spouse, dies, sells, or permanently
moves out of the home. Contact Montana Housing at 800-761-6264 for the current rate
for a reverse mortgage and added details about the program.
To qualify for a reverse mortgage in 2024:

Photo: Adobe Stock
- A person must be 68 years of age or older.
- The home must be in Montana.
- The borrower(s) must be the owner(s) and occupant(s).
- Family income cannot exceed the following:
- 1 person household $30,120
- 2 person household $40,880
- 3+ person household $51,640
Before the loan process can begin, the applicant must meet with an approved reverse
mortgage counselor. The counselor can help a family decide whether a reverse
mortgage is best for their circumstances. More information
about the Montana Reverse Mortgage program is available
online, https://commerce.mt.gov/Housing/Homeownership/Reverse-Annuity-Mortgages.
A farmer or rancher should be aware that a reverse mortgage loan must be paid off
before the home can pass to heirs.
Example: One rancher plans to leave the family home to his two daughters. But neither daughter has the funds to pay off the reverse mortgage. While the younger daughter wants to live in the home, it must be sold to pay off the reverse mortgage.
VETERANS’ BENEFITS
The Veteran’s Administration (VA) provides healthcare services for veterans with Alzheimer’s
or related dementias. Depending on the veteran’s needs, services may include home-based
care, homemaker and home health aides, respite care, adult day health care, outpatient
clinic, inpatient hospital, nursing home, palliative care, or hospice care. Caregiver
support is also an essential part of VA services.
The VA covers long-term care services under standard health benefits for those enrolled
in VA Health Care. The veteran may still need to pay a copay for other covered services.
More information about VA benefits is available online at https://www.va.gov/resources/does-va-cover-nursing-home-assisted-living-or-other-long-term-care/.
FUNDS FROM FAMILY
Some farmers and ranchers say they plan to depend on their adult children to pay for
long-term care costs if needed. However, this expectation can create financial hardships
for family members who are paying their own bills, saving and spending for their children’s
college education, saving for retirement, and making mortgage payments on their own
home, family farm, ranch, or other business. Unless there is a contractual agreement
between parents and children, Montana law does not require adult children to pay for
their parents’ long-term care costs.
Summary
Montana farmers and ranchers who make long-term care plans are more likely to have
an estate to leave to family members because they are less likely to use all their
financial resources to pay for the cost of long-term care. Planning for long-term
care costs also means less emotional and financial stress for everyone when the need
for long-term care arises because of the progression of Alzheimer’s. Setting up a
plan allows farmers and ranchers and their caregivers to access information that can
better prepare them for the future.
Legal Documents: Financial, Health, and Estate
PREPARING LEGAL DOCUMENTS IS AN IMPORTANT step to address at the beginning stages of an Alzheimer’s diagnosis while the person
has sufficient mental capacity for decision-making. A farmer or rancher in the early
stages of Alzheimer’s can still complete legal documents to ensure their family knows
their financial, health, and legacy planning wishes. After completing the proper legal
documents, they can then focus on enjoying life.
Current legal documents
The first step is to find, review, and consider whether any legal documents need updating.
If a Will or other legal documents have not been reviewed in the last five years,
take the time to make sure they reflect current wishes.
Make an appointment to meet with an attorney to learn what documents are necessary
when a family member has Alzheimer’s. After these legal documents have been completed
and signed, keep the originals in a safe but accessible place. Then, inform other
family members where they can be found.
Financial legal documents
FINANCIAL POWER OF ATTORNEY
As soon as family members suspect Alzheimer’s or when a physician has made an early
diagnosis, a financial power of attorney should be completed. The person who has Alzheimer’s
needs to sign the document while they have sufficient legal capacity.
A financial power of attorney is a legal document that a person (called the principal)
uses to appoint another person (called an agent) to manage the principal’s finances
and property. The agent pays the bills, deposits money in bank or credit union accounts,
and runs the farm or ranch business if the principal cannot. In Montana, a power of
attorney is durable, which means it is effective even if the principal becomes incapacitated
unless the principal states otherwise in the document.

Photo: Adobe Stock
Montana’s Uniform Power of Attorney Act provides safeguards and provisions for creating
and using a statutory form for a power of attorney. The Act lists the agent’s duties
and specific authority, including a section, “Important Information for Agent,” which
describes an agent’s duties as a fiduciary.
A fiduciary is someone who acts on behalf of another individual. The agent must act
in the best interest of the principal. In addition, the Act outlines potential liability
for any losses caused by an agent’s violations. This includes any actions the agent
takes outside the authority the principal has given the agent. Circumstances for ending
an agent’s authority are included as well.
Example: Ruby, a farm widow who showed signs of Alzheimer’s but still has legal capacity,
named her son, Ron, as an agent in her financial power of attorney. Unfortunately,
Ron used money in Ruby’s savings account to buy himself a car and take a trip to Las
Vegas. Ron is in violation of the Act. The successor agent, Ruth’s daughter, successfully
sued Ron and recovered the money he misused. Because Ruby still had legal, mental
capacity at the time, she had her attorney prepare a new power of attorney naming
Ruby’s daughter as agent.
Have a detailed conversation with a potential agent about the farm and ranch financial
responsibilities expected of the person, as the agent, to perform. The person should
be very trustworthy. Ask whether the person is willing to assume the duties and responsibilities
outlined in the Act. If the person says no, consider who among family and friends
would be a desirable next choice for an agent. Be sure to name a successor agent in
case the original agent is unavailable, resigns, dies, or is unwilling to serve.
MSU Extension has a MontGuide describing the requirements for a Power of Attorney (financial). A copy can be requested from a local MSU Extension office or downloaded online,
https://store.msuextension.org/Products/Power-of-Attorney-(financial)-MT199001HR__MT199001HR.aspx. MSU Extension also has two forms available online for the Statutory Financial Power of Attorney and Agent’s Certification as to the Validity of Power of Attorney and Agent’s Authority, at www.montana.edu/estateplanning/powerofattorneyagentcertificationforms.pdf.
Health care and end-of-life legal documents
Health care decisions are personal. They are based on family and life experiences,
spiritual and religious beliefs, and knowledge gained throughout life. A person may
have shared feelings about medical and end-of-life issues with healthcare providers,
family, and friends. However, talking is not enough when the time arrives for making
decisions about health care and end-of-life issues. Written legal documents about
health care preferences ensure a person’s wishes are known by those making decisions
on their behalf.
The health care power of attorney is a separate document from a financial power of attorney.
HEALTH CARE POWER OF ATTORNEY
Powers of attorney for health care allow Montanans to name an agent to make health
care decisions for them if they are no longer able. These decisions could include
selecting a physician or other health care providers, types of treatments, and if
long-term care is needed, what type of facility is chosen.
Members of five organizations collaborated to develop a model form for a Montana Health Care Power of Attorney. The model form and related documents
are available in a booklet from MSU Extension, Health Care Power of Attorney and Related
Documents for Montanans, www.montana.edu/estateplanning/documents/hoafillableform.pdf.
The booklet includes a worksheet designed to raise questions that, when answered,
will help an agent and family members make decisions about health care and preferences
for end-of-life treatments. Consider completing the worksheet before appointing a
health care agent.
The Health Care Power of Attorney includes a Living Will or a declaration (the term
used in Montana). This form notifies the health care agent and healthcare providers
about preferences for withholding or withdrawing life-sustaining treatments. It satisfies
the requirements of the Montana Rights of the Terminally Ill Act. A fact sheet and
form are available from MSU Extension, https://store.msuextension.org/Products/Health-Care-Power-of-Attorney-and-Related-Documents-for-Montanans-EB0231__EB0231.aspx.
Finally, the Health Care Power of Attorney booklet includes a form that, when completed, informs the agent and family members
about spiritual or religious preferences. This form can guide the agent and family
about decisions concerning the disposition of the body under the Montana Right of
Disposition Act. For detailed information, access the MSU Extension MontGuide, What
Are Your Rights Over Your Remains?, https://store.msuextension.org/Products/What-Are-Your-Rights-Over-Your-Remains-MT200918HR__MT200918HR.aspx.
Provider Orders for Life-Sustaining Treatment (POLST)
A POLST is a standardized medical order form with a list of specific types of life-sustaining
treatments a person does or does not want if the person is seriously ill and cannot
make those decisions. Montana healthcare providers have copies of the form available
for patients. A physician, nurse practitioner, or physician assistant will go through
the POLST form with a patient.
As a medical order, a POLST becomes a part of the health care records. After a POLST
form is signed by the patient and physician or nurse practitioner, Montana healthcare
providers will honor it. If a person has signed a Living Will or a health care power
of attorney addressing desires about medical treatment near the end of life, as well
as a POLST, they should all be reviewed for consistency. MSU Extension has a MontGuide
describing POLST and a sample form, https://store.msuextension.org/publications/HomeHealthandFamily/MT201112HR.pdf.
Estate planning legal documents
A WILL
A Will is a written document describing how its maker (called testator in Montana)
wants personal and real property distributed after death. By making a Will, a person
decides who receives farm or ranch property, what percentage of an estate each beneficiary
receives, and when each beneficiary receives assets. MSU Extension has a MontGuide
with more information on Wills, https://store.msuextension.org/publications/FamilyFinancialManagement/MT198906HR.pdf.
One concern about Alzheimer’s and the validity of a Will is, “What was the individual’s
legal capacity when signing the Will?” In general, a person must have a sound mind.
Sound mind means the testator (the person who makes the Will) knows the property the
testator owns and who will receive the property upon the testator’s death. A farmer
or rancher may have sufficient legal capacity to make a Will, even though the person
is elderly, intellectually challenged, or in the early stages of Alzheimer’s.
Courts recognize that people have good and bad days. An individual who shows early
signs of Alzheimer’s, such as repeating questions, getting lost while driving, or
having difficulty with everyday tasks, could still have enough legal mental capacity
in the morning to sign a Will. However, the same person may lack legal mental capacity
in the afternoon or evening.

Photo: Jane Wolery
Separate List Referred to in a Written Will
Montana’s Uniform Probate Code has a provision allowing a person to refer to a “separate
list” in a Will. The personal representative (PR) uses the list to distribute tangible
personal property to beneficiaries. Examples of such items include family photographs,
rodeo belt buckles, saddles, boots, or a pie plate that has special meaning for the
person making the list and other family members, friends, or colleagues. These types
of personal possessions, as well as jewelry, stamps, gun and coin collections, or
quilts, are non-titled property because there are no legal documents (such as titles,
deeds, or signature cards) to show who owns the property.
This list does not appear in the body of the Will. The list is separate from it. A
provision in the Will says the person writing the Will has prepared such a list or
may prepare the list in the future. The list must describe the items and name the
person who is to receive each item.
Example: “To my son, Rex Jones, my collection of National College Rodeo Belt Buckles.”
Mr. Jones makes it clear that he wants the National College Rodeo Belt Buckles to
pass to his son Rex Jones and not to another Rex Jones who lives in the same county.
A person may update the list as needed without having to change the Will.
More information is in the MSU Extension MontGuide Who Gets Grandma’s Yellow Pie Plate? Transferring Non-Titled Property, https://store.msuextension.org/publications/FamilyFinancialManagement/MT199701HR.pdf.
The person writing a Will cannot use the separate list to distribute money in checking
or savings accounts because these are titled accounts. If a checking or savings account
is solely owned, a person can make a payable on death designation (POD) on it. A transfer
on death registration (TOD) is the tool to name beneficiaries for stocks, bonds, and
mutual funds. More information is in the MSU Extension MontGuide Nonprobate Transfers, https://store.msuextension.org/publications/FamilyFinancialManagement/MT199509HR.pdf.
In a Will, a testator should nominate someone to administer the testator’s estate
(called personal representative [PR] in Montana). After the testator’s death, the
nominated PR must complete an application for court appointment. The PR applicant
acknowledges the PR is a fiduciary and has obligations to the testator’s estate and
its beneficiaries. The PR applicant must also recognize that no property or other
assets of the testator’s estate can be used for the PR’s personal benefit. The “Acknowledgement
of Fiduciary Relationship and Obligations Personal Representative, Guardian, or Conservator”
form listing these fiduciary relationship statements is available online from MSU
Extension, www.montana.edu/estateplanning/acknowledgementoffiduciaryrelationship.pdf.
MSU Extension also has a MontGuide outlining the Personal Representative Responsibilities, https://store.msuextension.org/publications/FamilyFinancialManagement/MT199008HR.pdf.
Trusts
Although trusts have existed for years, they have recently gained more visibility.
There may be advertisements for free seminars on the benefits of trusts. Or a local
coffee group member may have shared how trusts have solved some estate planning problem.

Photo: Melissa Ashley
Legitimate educational seminars on trusts and other legal and financial topics are sometimes offered by MSU Extension, attorneys, financial planners and trust officers from banks and trust companies. Understandably, these professionals want to promote their expertise through these programs. There are some promoters, however, who may give a false impression that trusts can solve every estate planning and financial problem imaginable.
Definitions of the meaning of words used in a trust document are below.
- A trust is a fiduciary arrangement that requires its trustee to hold assets for the benefit of the beneficiary.
- A settlor is a person who sets up a trust.
- A trustee is a person, bank, or trust company chosen by the settlor to manage and distribute the trust assets. According to the trust instrument and Montana law, the trustee must consider what is in the beneficiary’s best monetary interests.
- A trustee is a fiduciary who manages money or property for another person and not for the benefit of the trustee.
TESTAMENTARY TRUST
A farmer or rancher may create a testamentary trust in a written Will. The Will includes
the terms of the trust, such as defining the trust beneficiaries, the trustees and
successor trustees, the standards for the distribution of assets from the trust to
the beneficiaries, when the trust ends, and any other special directions.
After a person dies, typically a family member or an attorney delivers the Will to
the clerk of the district court to start the probate process. Probate is the legal
transfer and administration of estate assets owned by a deceased person.
A testator’s Will provides which assets pass to a testamentary trust. Those assets
could include the testator’s farm or ranch land, house, money in checking and savings
accounts, stocks, bonds, mutual funds or all the testator’s real and personal property.
In addition, life insurance proceeds, annuity payments, and pensions may allow a policyholder
to list a testamentary trust as the beneficiary to receive the proceeds. Check with
each company’s policy to learn if this beneficiary option is available.
For more information, read the MSU Extension MontGuide Testamentary Trusts in Montana, https://store.msuextension.org/publications/FamilyFinancialManagement/MT202113HR.pdf.
 Photo: Melissa Ashley
Photo: Melissa Ashley
REVOCABLE TRUST
A revocable trust allows a settlor, while alive, to set up a trust to hold assets
for eventual distribution to beneficiaries. A settlor decides which farm or ranch
property to include in the revocable trust.
A settlor must change the title of ownership of each asset to be placed in the trust
from the settlor’s name to the trust’s name. Merely signing a trust agreement does
not place property in the trust. A farmer or rancher should meet with an attorney
who can explain the benefits of a revocable trust, such as avoiding probate after
the settlor’s death.
Typically, settlors name themselves as the original trustee of a revocable trust.
Or, the settlor may name another person, such as a family member, friend, or a bank/trust
company to serve as a trustee or as a successor trustee.
The farmer or rancher can change the terms of the trust or end it completely at any
time. That is why the trust is referred to as a revocable trust. The trustee manages
trust assets for the benefit of the settlor while the settlor is alive. The trustee
pays bills and makes other financial decisions about the trust assets.
Upon the settlor’s death, the trustee manages trust assets for the benefit of the
trust beneficiaries named in the trust document. The trust document could say the
trust continues after the settlor’s death with the funds used to care for a spouse.
Or, it may say the trustee is to distribute all trust assets to the spouse, children,
or other beneficiaries upon the settlor’s death.
Make an appointment with an attorney who can help decide if a revocable trust is right
for a farm or ranch situation. For background information about revocable trusts,
read the MSU Extension MontGuide Revocable Living Trusts, https://store.msuextension.org/publications/FamilyFinancialManagement/MT199612HR.pdf.
Finally, the MSU Extension MontGuide Financial, Estate, and Health Care Planning Documents for Montanans Concerned About
Memory Loss discusses how Alzheimer’s has affected people in different situations and the legal
documents attorneys recommend, https://store.msuextension.org/publications/FamilyFinancialManagement/MT202005HR.pdf.
Summary Family members, friends, caregivers, and others can protect the financial health of
a farmer or rancher living with Alzheimer’s by helping the farmer or rancher consider
and sign legal documents when the farmer or rancher has sufficient mental capacity
to do so.
Family members, friends, caregivers, and others can protect the financial health of
a farmer or rancher living with Alzheimer’s by helping the farmer or rancher consider
and sign legal documents when the farmer or rancher has sufficient mental capacity
to do so.
MSU Extension has three MontGuides informing individuals how to place beneficiary
designations on personal and real property without the cost involved in probate.
- Transfer on Death Deed for real property (TODDs).
- Payable on Death Designations on savings and checking accounts, and certificates of deposit (PODs) and Transfer on Death Registrations for stocks, bonds, and mutual funds (TODs).
- Montana Motor Vehicle Beneficiary Designation Form (MV13) for vehicles and vessels (for example: boat, personal watercraft and motorized pontoon).
The MontGuides are available online at www.montana.edu/estateplanning/eppublications.html.
Photo: Adobe Stock
Helping Children Understand Alzheimer's
IN MONTANA, THERE ARE MORE THAN 17,000 family caregivers for people with Alzheimer’s.
Many are caring for someone with the disease and caring for a child or grandchild
at the same time. Thus, we have children across the state who may be experiencing
and interacting with someone, such as a grandparent,* with Alzheimer’s.
What do children experience with a grandparent living with Alzheimer’s?
A grandparent living with Alzheimer’s often repeats stories, asks the same questions
over and over, and can become easily agitated or express paranoia. They may wander
on the farm or ranch property, get disoriented, and be unable to find their way home.
In a later stage, a grandparent may not know where they live, nor recognize family
members. These changes can upset a child and be difficult to understand.
As a family caregiver’s role becomes more demanding, a young child may experience
a wide range of emotions. Acknowledging the child’s feelings and experiences and explaining
what is causing the grandparent to act differently is important.
Alzheimer’s symptoms and the added demands they create for families can negatively
affect a child’s emotions and behaviors. As a result, a child may decide to spend
less time with the family member or become emotionally detached. When with a grandparent,
they may become anxious, scared, and upset. If the grandparent lives with the family,
a child may experience these emotions often and may be embarrassed to have friends
around.
Changes in mood, personality, and behavior in a grandparent with Alzheimer’s can be
particularly upsetting to a child who lacks knowledge about the disease. Family members
who are well-informed can help a child understand the changes. A child needs age-appropriate
information about Alzheimer’s, its symptoms and its progression. A child can learn
effective ways to relate to their grandparent.
Explain to the child that Alzheimer’s is not a part of normal aging and that it is
a serious medical condition. When a family caregiver has adequate and correct information
about this form of dementia, they can provide family members with the necessary support
needed to understand the disease.
Storybooks portraying a child’s experiences with a grandparent who has Alzheimer’s
may help the child understand the disease. Talking with a child about what is happening
in a story and focusing on the child’s reactions supports a child’s social and emotional
well-being.
* While the word “grandparent” appears extensively in this article, the information
applies whether the person with Alzheimer’s is another relative, neighbor, or family
friend.
What is developmental bibliotherapy?
Developmental bibliotherapy uses storybooks to support social, emotional, and cognitive
well-being and growth in children. Storybooks have been shown to help a child with
life’s transitions. Storybooks provide children with characters they can connect with.
This connection can
help them understand and cope with complicated situations.
Storybooks can give the adult reader a deeper understanding of what a child is experiencing.
They can provide ideas for helping a child with their emotions and relationships.
Multigenerational families can develop stronger relationships when they work together
to care for the person with Alzheimer’s.
Storybooks depicting families’ experiences with Alzheimer’s can be effective for helping
children to:
- Learn about and relate to an issue or problem they are experiencing.
- Recognize, understand, express, and manage the feelings they have toward their grandparent and their experiences.
- See, learn, develop, and integrate social skills modeled by characters in the storybook.
- Explain, from their perspective, behaviors they see their grandparent display.
- Explore healthy approaches to problems or situations experienced by the child and family.
- Gain ideas for helping their grandparent.
Research reveals that after reading and discussing storybooks, children and adults
experience an increase in positive attitudes. They are more willing to interact with
a family member who has Alzheimer’s.
Where to find storybooks about Alzheimer’s
Storybooks about Alzheimer’s for children of all ages are available from a variety
of sources:
- Montana State University Extension has a website with reading guides for storybooks, Using Storybooks to Teach Children and Adults About Alzheimer’s, https://www.montana.edu/extension/alzheimers
- The Alzheimer’s Association has a five-page handout listing Books for Kids and Teens with the age level, title, and description, online, www.alz.org/media/documents/books-for-kids-teens-rl-2015.pdf.
- The Alzheimer’s Foundation of America sells two storybooks recommended for children
ages five to eight. Call 866-232-8484 to order, or online, https://shop.alzfdn.org
- Dancing with Granddad: An Alzheimer’s Story for Children and their Families
- Gardening with Grandma: An Alzheimer’s Story for Children and their Families
- A local library or a nearby bookstore may have storybooks about Alzheimer’s for children.
- Another source for Alzheimer’s storybooks is online. However, selecting a storybook for children may seem overwhelming. Try searching with the phrase: children’s storybooks about Alzheimer’s. Websites may list, for example, “Six children’s storybooks about Alzheimer’s disease and dementia,” or “the best children’s picture books about dementia.” Recurring recommendations suggest a storybook may be worth buying. An online search may include previews to help find a book with a theme that matches the child’s current experience with Alzheimer’s.
What to look for in an Alzheimer’s storybook
Regardless of where a storybook is found, read the description to see if the storybook
appears to:
- Support and preserve relationships between family members.
– For example, while a grandparent’s behaviors may change, there will always be the child’s love for the grandparent and the grandparent’s love for the child. - Focus on the specific issue or problem a child is experiencing. Examples include:
- A grandparent may be showing signs of forgetfulness and cannot remember the grandchild’s name.
- Grandma is crying because she wants to go home when she is already at home.
- Grandpa and his grandchild take walks around the ranch. Soon it is clear to the child that Grandpa does not know the way home. The child learns to tell him, “I am a scout and will get us home.”
- Match the goals for increasing understanding when reading a storybook about Alzheimer’s.
- The story reassures a child their grandparent still loves them.
- The story shares how a child can help their grandparent.
Then answer these questions to evaluate and select a storybook to help a child understand Alzheimer’s.
- Does it give straightforward, but not overwhelming information?
- Does it have relatable characters?
- Does it capture a child’s experiences with their grandparent?
- Does it show support from a parent or caregiver for a child?
- Do the characters portray positive modeling, healthy coping skills, and positive communication?
- Does the person in the storybook with Alzheimer’s show common behaviors like a child is experiencing?
- Does it show supportive relationships between the child and the grandparent?
- Is the child in the storybook positively involved in the grandparent’s life?
Guidelines to follow when reading to a child
Researchers have created guidelines to make reading a storybook to a child more effective.
By following these guidelines, better learning outcomes and a more
enjoyable experience can be achieved.
Stick to a schedule. A schedule helps a child know what to expect. A consistent schedule to read together
gives quality time for reader and child. Ask:
- Is there a quiet time in the day when I will not be preoccupied?
- What are possible distractions? For example: Is the child hungry? Is the child’s favorite cartoon on? Is the child too tired? Is the child upset because of something their grandparent said or did?
Keep the child involved during reading. A child is likely to build mental pictures of what they hear. They may express thoughts
and ask questions. As the reader, point out important parts of the story. This supports
the child’s reading and language skills.
Ask questions before and while reading. Ask a child:
- “What just happened?”
- “What do you think is going to happen next?”
- “What do you think the little girl should do to help her Grandma?”
- "How could the little boy help Grandpa find his way to the garden?”
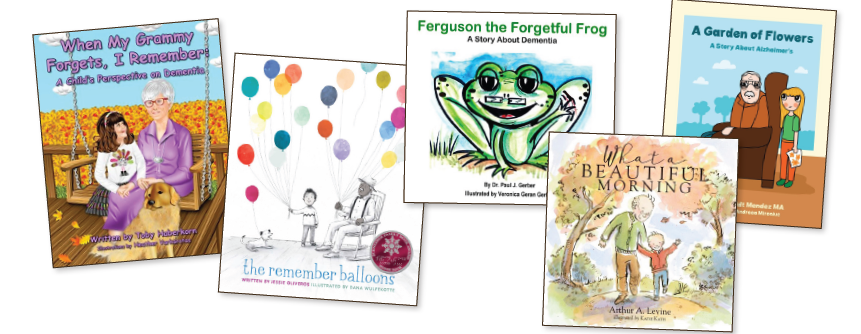
Is the child able to interact and answer questions? If not, simplify them.
- “How could the little boy help Grandpa find his wallet?”
- What can the little girl do if Grandma tries to go outside in the winter without shoes and a coat?”
 Answer the child’s questions. This supports a child’s in-depth learning and increases their understanding of a
storybook’s main concepts. If a response to a child’s question is difficult, look
up the answer together or follow up with the child later. Answering a child’s questions
with patience fosters curiosity. It also helps the child realize it’s acceptable to
ask questions about a grandparent’s behavior.
Answer the child’s questions. This supports a child’s in-depth learning and increases their understanding of a
storybook’s main concepts. If a response to a child’s question is difficult, look
up the answer together or follow up with the child later. Answering a child’s questions
with patience fosters curiosity. It also helps the child realize it’s acceptable to
ask questions about a grandparent’s behavior.
Read the storybook multiple times. Repetition increases learning. It supports a child’s understanding of stories, helps
build reading and language skills, and is a part of their development. A child may
notice different aspects of the story each time the storybook is read.
Is the storybook too long for the child? If there isn’t time to read the whole book in one sitting, be sure to review the
part of the story already read to the child before another reading session. The recap
will help the child transition into the remaining story.
What if a child does not like the story? Try changing voice to fit the characters. Adjust tone to express emotions of the
story. Or, read the storybook at a different time of day. If these strategies do not
work and the child still does not like it, find another storybook about Alzheimer’s.
Photo: Adobe Stock
MSU Extension offers a free storybook for Montanans
A storybook about Alzheimer’s is available without charge to Montana parents, grandparents,
and others who would like one to read to a child. Complete the form on the following
website and type “Alzheimer’s Storybook 1” in the code box: www.montana.edu/extension/alzheimers/alzheimersfreestorybookorderform.html.
Montana residents who do not have computer access can send their name, address, and
the code “Alzheimer’s Storybook 1” to Marsha Goetting, P.O. Box 172800, Bozeman, MT
59717 to receive a free book.
Funding of the MSU Extension Alzheimer’s Storybook program
The authors express appreciation to AARP Montana and the University of Montana Geriatric
Education Center for providing funds to buy storybooks for caregivers with children.
They are helping Montanans who want their children to understand and develop empathy
towards someone with Alzheimer’s disease.
The authors also express appreciation to members of the Montana Alzheimer’s and Related
Dementias Coalition and MSU Extension agents for their contributions to reading guides,
www.montana.edu/extension/alzheimers/booksandreadingguides.html.
Parting Words
WORKING IN ISOLATION AND LIVING IN MONTANA’S rural communities creates a need for education about Alzheimer’s specific to farm
and ranch operations. This primary reason encouraged authors to write articles for
Volumes 1 and 2 of this magazine. They wanted to provide helpful information to Montanans
with Alzheimer’s and their caregivers.
Empowering farm and ranch families to recognize the early signs of Alzheimer’s and
to ensure the safety of the person who is living with Alzheimer’s were two specific
purposes. Another was to enable caregivers to know the vital importance of self-care
for their physical, mental, and emotional health.
A very recent discovery in diagnosing Alzheimer’s is a blood test for a specific blood
biomarker, the p-tau217 blood test. The test is reported to accurately diagnose 90
percent of early Alzheimer’s cases. An amyloid PET scan and a p-tau217 test are the
current gold-standard scientific methods, other than an autopsy, for identifying Alzheimer’s.
Both tests are expensive, invasive, and are not readily available across the United
States, according to experts. The authors will continue to keep abreast of new research
into the causes and prevention of Alzheimer’s and share updates to support Montanans
living with Alzheimer’s and their caregivers.

Photo: Peter Kolb
REFERENCES
Alzheimer’s and Driving: Concerns and Decisions
- Alzheimer’s Association. 2024. Dementia and Driving. www.alz.org/help-support/caregiving/safety/dementia-driving
- Alzheimer’s Society of United Kingdom. 2024. Driving and Dementia. www.alzheimers.org.uk/get-support/staying-independent/driving-dementia
- Bell, Matt. May 2023. Driving & Dementia/Alzheimer’s: State Laws, Coping & Advice for Caregiver. www.dementiacarecentral.com/caregiverinfo/driving-problems
- DailyCaring. 2024. 8 ways to stop an elderly person from driving when all else fails. https://dailycaring.com/8-ways-to-stop-an-elderly-person-from-driving-when-all-else-fails
- Dementia Action Collaborative Washington State. January 2020. Safety Concerns for People with Dementia. https://familymedicine.uw.edu/cpc/wp-content/uploads/sites/15/2021/09/Dementia-Safety-Informational-Toolkit.pdf
- Family Caregiver Alliance. 2002. Dementia and Driving. www.caregiver.org/resource/dementia-driving
- Fisher Center for Alzheimer’s Research Foundation. September 2021. Erratic Driving as an Early Indicator of Alzheimer’s Disease. www.alzinfo.org/articles/diagnosis/erratic-driving-as-an-early-indicator-of-alzheimers-disease
- Hartford Center. 2024. Understanding Dementia & Driving. www.thehartford.com/resources/mature-market-excellence/dementia-driving
- Harvard Health Publishing, Harvard Medical School. October 2022. What’s the relationship between memory loss and driving?www.health.harvard.edu/blog/whats-the-relationship-between-memory-loss-and-driving-202210122829
- National Institute on Aging. April 2023. Driving Safety and Alzheimer’s Disease. www.nia.nih.gov/health/driving-safety-and-alzheimers-disease
- Sparks, Dana. November 2019. Alzheimer’s and dementia: When to stop driving? Mayo Clinic News Network. https://newsnetwork.mayoclinic.org/discussion/alzheimers-and-dementia-when-to-stop-driving
Wandering: A Safety Concern
- Alzheimer Society of Canada. 2024. Wandering and dementia. https://alzheimer.ca/bc/en/help-support/programs-services/dementia-resources-bc/wandering-disorientation-resources/wandering-dementia
- Alzheimer’s Association. 2024. Wandering. www.alz.org/help-support/caregiving/stages-behaviors/wandering#:~:text=
- Alzheimer’s Association. January 2023. Wandering and getting lost: Who’s at risk and how to be prepared. www.alz.org/media/documents/alzheimers-dementia-wandering-behavior-ts.pdf
- Alzheimer’s Foundation of America. 2023. Dementia and Wandering: Reducing the Risks.https://alzfdn.org/wandering-and-demenita
- Barnard-Brak, L. Richman, D. Own D. July 2018. Assessing wandering risk among individuals with Alzheimer’s Disease and Dementia: A Pilot Study. Psychogeriatrics. https://onlinelibrary.wiley.com/doi/abs/10.1111/psyg.12336
- Bright-Focus Foundation. August 2021. How to Prevent Wandering in Alzheimer’s Patients. www.brightfocus.org/alzheimers/article/how-prevent-wandering-alzheimers-patients
- Cipriani, G., C. Lucetti, A. Nuti, and S. Danti. 2014. Wandering and dementia. Psychogeriatrics. https://onlinelibrary.wiley.com/doi/full/10.1111/psyg.120443
- Cleveland Clinic Health Essentials. September 2022. What to do when someone with Alzheimer’s Disease wanders. https://health.clevelandclinic.org/what-to-do-when-alzheimers-patients-wander
- National Institute on Aging. 2017. Coping with Alzheimer’s Behaviors: Wandering and Getting Lost. www.nia.nih.gov/health/wandering-and-alzheimers-disease
- Schmall, V., S. Bowman, and C. Pratt. 2020. Helping Memory-Impaired Elders: A Guide for Caregivers. Oregon State University. https://extension.oregonstate.edu/catalog/pub/pnw-314-helping-memory-impaired-elders-guide-caregivers
- Sparks, D. 2020. Mayo Clinic News Network. Alzheimer’s and dementia: Understand wandering and how to address it.https://newsnetwork.mayoclinic.org/discussion/alzheimers-and-dementia-understand-wandering-and-how-to-address-it
- University of Pittsburg Medical Center. 2024. Wandering in Patients with Alzheimer’s Disease and Dementia.www.upmc.com/services/seniors/resources-for-caregivers/wandering-tendencies-patients-alzheimers-dementia
Safety Measures in the Home and Surrounding Environment
- Aging Resources of Central Iowa. August 2010. Home Safety for People with Alzheimer’s Disease. www.agingresources.com/wp-content/uploads/2015/04/home_safety_for_people_with_alzheimers_disease-1.pdf
- Alzheimer’s Association. Home Safety. 2024. www.alz.org/help-support/caregiving/safety/home-safety
- Alzheimer’s.gov. May 2024. Tips for Caregivers and Families of People with Dementia. www.alzheimers.gov/life-with-dementia/tips-caregivers
- Alzheimer’s Society of United Kingdom. 2020. Keeping Safe at Home. www.alzheimers.org.uk/get-support/staying-independent/keeping-safe-home
- Cleveland Clinic. December 2023. How to Care for Someone with Alzheimer’s Disease. https://health.clevelandclinic.org/alzheimers-caregiver-tips
- Jepsen, S.D. November 2013. Ohio AgrAbility Fact Sheet Series. Farming with Alzheimer’s Disease. https://ohioline.osu.edu/factsheet/AEX-982.9
- Johns Hopkins Medicine. 2024. Dementia Care: Keeping Loved Ones Safe and Happy at Home. www.hopkinsmedicine.org/health/wellness-and-prevention/safe-and-happy-at-home
- Lynch, Mike. American Bar Association. March 2022. Home Safety for People Living with Dementia. www.americanbar.org/groups/senior_lawyers/publications/voice_of_experience/2022/march-2022/home-safety-for-people-with-dementia/
- Renown Health. 2022. Alzheimer’s Safety Tips for Caregivers to Know. www.renown.org/blog/alzheimers-safety-tips-for-caregivers-to-know
- Safe Ag Systems. 2023. Dementia Australia. The effects of dementia on farm life. www.safeagsystems.com/blog/dementia-farm-safety
- Van Dyk, Deirdre and Dono, Linda. November 2023. 50 Tips to Help Keep Dementia and Alzheimer’s Patients Safe in Your Home.
www.aarp.org/caregiving/home-care/info-2017/dementia-home-safety.html - Washington State Dementia Action Collaborative (DAC). February 2022. Safety Concerns for People with Dementia Info Kit. www.dshs.wa.gov/sites/default/files/ALTSA/stakeholders/documents/AD/Dementia%20Safety%20Information%20Toolkit.pdf
- WebMD. May 2023. Make Your Home Safe for Someone with Alzheimer’s. www.webmd.com/alzheimers/caregiving-preparing-home
Planning for the Cost of Long-Term Care
- Administration for Community Living, Administration on Aging. August 2021. Understanding Long-term Care. https://acl.gov/ltc/basic-needs
- Administration for Community Living. LongTermCare.gov. February 2020. How much care will you need?https://acl.gov/ltc/basic-needs/how-much-care-will-you-need
- Alzheimer’s Association. January 2023. Planning ahead for long-term care expenses. www.alz.org/media/Documents/alzheimers-dementia-plan-ahead-long-term-care-expenses-ts.pdf
- Annuity.org. January 2024. Long-Term Care Statistics to know in 2024. www.annuity.org/retirement/health-care-costs/long-term-care/statistics
- betternurse.org. July 2023. Understanding Skilled Nursing Facilities: What You Need to Know. https://betternurse.org/what-is-skilled-nursing-facility/
- Hoyt, Jeff. Seniorliving.org. March 2024. Nursing Home Costs in 2024. www.seniorliving.org/nursing-homes/costs
- Marcus, John. September 2022. AARP. Experts Urge Earlier Planning for Long-term Care. www.aarp.org/caregiving/financial-legal/info-2022/planning-for-long-term-care.html
- Masterson, Les. August 2023. Forbes Advisor. What is the Cost of Long-Term Care Insurance?www.forbes.com/advisor/life-insurance/long-term-care-insurance-cost
- Montana Department of Commerce. 2024. Montana Reverse Annuity Mortgage (RAM) program. https://housing.mt.gov/Homeownership/Reverse-Annuity-Mortgages
- Moore, R. April 2022. The Ohio State University Extension. Long-Term Care Costs: What are the odds?https://farmoffice.osu.edu/blog/wed-04202022-1047am/long-term-care-costs-what-are-odds#
- National Clearinghouse of Long-Term Care Information. January 2021. What is long-Term Care (LTC) and Who Needs It? https://LongTermCare.gov
- National Institute on Aging. October 2023. What is Long-term Care?www.nia.nih.gov/health/what-long-term-care#types
- National Institute on Aging. October 2023. Paying for Long-term Care. www.nia.nih.gov/health/long-term-care/paying-long-term-care
- National Institute on Aging. October 2023. Long-Term Care Facilities: Assisted Living, Nursing Homes, and Other Residential Care.www.nia.nih.gov/health/assisted-living-and-nursing-homes/long-term-care-facilities-assisted-living-nursing-homes
- Senior Guidance. 2024. Memory Care Facilities in Montana. www.seniorguidance.org/memory-care/montana
- U. S. Department of Veterans Affairs. November 2023. Dementia Care (including Alzheimer’s Disease). www.va.gov/GERIATRICS/pages/Alzheimers_and_Dementia_Care.asp
- U. S. Department of Veterans Affairs. October 2022. Does VA cover nursing home, assisted living, or other long-term care?www.va.gov/resources/does-va-cover-nursing-home-assisted-living-or-other-long-term-care/
Legal Documents: Financial, Health, and Estate
- Alzheimer’s Association. 2024. Legal Documents. www.alz.org/help-support/caregiving/financial-legal-planning/legal-documents
- Alzheimer’s Association. 2024. Legal and Financial Worksheet. www.alz.org/media/Documents/worksheet-financial-legal.pdf
- Alzheimer’s Association. 2024. Planning Ahead for Legal Matters. www.alz.org/help-support/caregiving/financial-legal-planning/planning-ahead-for-legal-matters
- Gaugler J., E. Jutkowitz, C. Peterson, and R. Zemora. December 2018. Caregivers dying before care recipients with dementia. Doi: 1016/j.trci.2018.08.010. www.ncbi.nlm.nih.gov/pmc/articles/PMC6292823/
- Montana Code Annotated. 2023. Part 3, Uniform Power of Attorney Act, §72-31-301 through §72-31-367. https://leg.mt.gov/bills/mca/title_0720/chapter_0310/part_0030/sections_index.html
- Montana Code Annotated. 2023. Part 5, Wills, Will Contracts, and Custody and Deposit of Wills, §72-2-501 through §72-2-537. www.leg.mt.gov/bills/mca/title_0720/chapter_0020/part_0050/sections_index.html
- Montana Code Annotated. 2023. Chapter 38, Montana Uniform Trust Code, Part 1 through Part 11. https://leg.mt.gov/bills/mca/title_0720/chapter_0380/parts_index.html
- Montana Code Annotated. 2023. Chapter 9, Rights of the Terminally Ill Act Part 1 – Part https://leg.mt.gov/bills/mca/title_0500/chapter_0090/parts_index.html
- Montana Code Annotated. 2023. Part 5, Health Care Power of Attorney Not Revoked Until Notice, §72-5-502. https://leg.mt.gov/bills/mca/title_0720/chapter_0050/part_0050/section_0020/0720-0050-0050-0020.html
- Montana Board of Medical Examiners. 2014. POLST, Provider Orders for Life-Sustaining Treatment. https://boards.bsd.dli.mt.gov/Portals/133/Documents/med/POLST/dli-bsd-pol002.pdf
Helping Children Understand Alzheimer’s
- Alzheimer Society of Canada. 2024. Helping children understand dementia. https://alzheimer.ca/en/help-support/i-have-friend-or-family-member-who-lives-dementia/helping-children-understand-dementia
- Alzheimer’s Disease in Fiction. 2024. Good Reads, Listopia. www.goodreads.com/list/show/16500.Alzheimer_s_Disease_in_Fiction
- Alzheimer’s Association. 2024. Alzheimer’s and dementia facts and figures. www.alz.org/alzheimers-dementia/facts-figures
- Alzheimer’s Association. 2023. Parent’s Guide: Helping Children and Teens Understand Alzheimer’s Disease. www.alz.org/documents/national/brochure_childrenteens.pdf
- Alzheimer’s Society. London England. How to talk about dementia with children and young people. www.alzheimers.org.uk/get-support/daily-living/how-talk-dementia-children-young-people
- Alzheimer Society of Canada. 2018. Resource List for Kids. https://alzheimer.ca/sites/default/files/documents/resource-list-for-kids.pdf
- Burress, H. Lotsa Helping Hands. 2024. How to Teach Children about Grandparents with Dementia. https://lotsahelpinghands.com/blog/how-to-teach-children
- Carpenter, B., S. Zoller, S. Balsis, P. Otilingam, & M. Gatz. 2011. Demographic and Contextual Factors Related to Knowledge About Alzheimer’s Disease.
American Journal of Alzheimer’s Disease and Other Dementias, 26(2), 121-126.
https://pubmed.ncbi.nlm.nih.gov/21233137/ - Frontier Senior Living. Helping children understand dementia and Alzheimer’s through fun activities with Grandparents. https://frontiermgmt.com/blog/helping-children-understand-dementia-alzheimers-through-fun-activities-with-grandparents/
- Hicks, K. 2018. Teaching children how to talk to senior loved ones with dementia. www.alzheimers.net/teaching-children-how-to-talk-to-loved-ones-with-dementia
- Holland, M. May 2005. Using Picture Books to Help Children Cope with a Family Member’s Alzheimer’s Disease. Young Children, 60(3), 105-109. https://eric.ed.gov/?id=EJ751375
- Magnuson, S. April 1999. Strategies to help students whose grandparents have Alzheimer’s disease. Professional School Counseling, 2(4), 327-333.
- National Institute on Aging. 2017. Helping Children Understand Alzheimer’s Disease. www.nia.nih.gov/health/helping-children-understand-alzheimers-disease
- Sakai, E. Y., B. D. Carpenter, & R. E. Rieger. September 2012. What’s wrong with Grandma? Depictions of Alzheimer’s disease in children’s storybooks. American Journal of Alzheimer’s Disease & Other Dementias, 27(8), 584-591. https://journals.sagepub.com/doi/10.1177/1533317512459796
- Sulzenko, J. C. 2024. Discussion Guide for the play: What my Grandma means to say. https://jcsulzenko.com/books/what-my-grandma-means-to-say/the-discussion-guide
- Werner, P. 2001. Correlates of family caregivers’ knowledge about Alzheimer’s disease. International Journal of Geriatric Psychiatry, 16(1), 32-38.
Copyright © 2024 MSU Extension
We encourage the use of this document for nonprofit educational purposes. This document
may be reprinted for nonprofit educational purposes if no
endorsement of a commercial product, service or company is stated or implied, and
if appropriate credit is given to the author and MSU Extension. To use
these documents in electronic formats, permission must be sought from the Extension
Communications Director, 135 Culbertson Hall, Montana State University, Bozeman, MT
59717; E-mail: publications@montana.edu
The U.S. Department of Agriculture (USDA), Montana State University and Montana State
University Extension prohibit discrimination in all of their programs
and activities on the basis of race, color, national origin, gender, religion, age,
disability, political beliefs, sexual orientation, and marital and family status.
Issued
in furtherance of cooperative extension work in agriculture and home economics, acts
of May 8 and June 30, 1914, in cooperation with the U.S. Department of
Agriculture, Cody Stone, Director of Extension, Montana State University, Bozeman,
MT 59717.
Resources and references listed or excluded do not imply endorsement or non-endorsement.


